Introduction: Severe forms of COVID-19 caused by SARS-CoV-2 have been observed in children with hematological malignancies. Occurrence of the infection during treatment may significantly delay chemotherapy, potentially exposing patients to a higher risk of relapse. Hence, the timely administration of SARS-CoV-2 vaccines represents a compelling preventive strategy. The PACIFIC trial (NCT04969601) aimed to explore the efficacy and tolerance and of SARS-CoV-2 vaccination in these patients population, at a time when the vaccine was not yet approved for children below the age of 12 years.
Methods: A phase I-II dose-finding study was conducted from 2021 to 2023 to assess the efficacy and tolerance of two doses of the BNT162b2 vaccine administered 21 days apart in children with acute leukemia (aged 1 to 15 years) and their siblings (aged ≥ 5 to 15 years). Children with acute lymphoblastic leukemia (ALL) received vaccination during maintenance treatment or within 12 months of treatment discontinuation and children with acute myeloblastic leukemia (AML) were vaccinated within 12 months of treatment discontinuation. For patients under the age of 12 years, a dose escalation using a Bayesian dose escalation scheme (10, 20, or 30 µg) was conducted. Tolerance was assessed by dose-limiting toxicity (DLT), which was defined as the presence of a grade 3 or higher adverse event attributable to the vaccine within 7 days of vaccination. The efficacy end-point was an anti-Spike IgG titer ≥ 260 BAU/ml at 2 months after the first injection. If this criterion was not met, a third vaccine dose was administered. Neutralizing anti-Spike IgG antibodies were assessed. Humoral response was studied at 0, 2 and 6 months after the first vaccine injection. The T-cell specific response was also tested by ELISpot at the same time points.
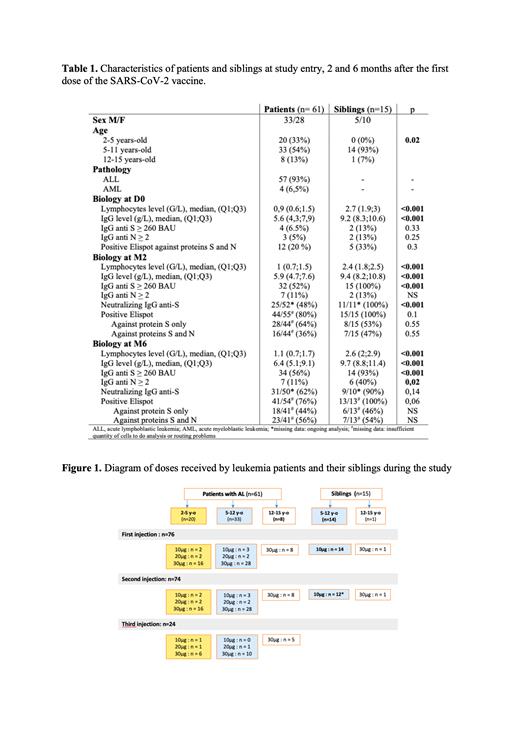
Results: Seventy-six children (61 patients and 15 siblings) were included in the study. Characteristics of children at the study entry, 2 and 6 months after the first dose of the SARS-CoV-2 vaccine are summarized in Table 1. No DLT was reported during the dose escalation phase therefore most children received a 30µg vaccine dose ( Figure 1). No vaccine-related serious adverse events were reported. Two months after the first injection, 32 (52%) patients and 15 (100%) siblings showed an anti-Spike IgG titer ≥ 260 BAU/ml. Approximately half (25/52,48%) of the patients and all (11/11) siblings had neutralizing antibodies. Most (44/55,80%) patients and all (15/15) siblings had a significant T-cell response against CoV2-protein S. Humoral response was significantly different in patients in comparison to siblings (p<0,001) whereas T-cell response was equivalent in the two groups (p=0.1). Twenty-four patients (39%) received a third dose. Forty-three percent achieved an anti-Spike IgG titer ≥ 260 BAU/ml one month after. Six months after the first injection, 34/61 (56%) patients and 14/15 (93%) siblings had still an anti-Spike IgG titer ≥ 260 BAU/ml. Most evaluable patients (31/50,62%) and siblings (9/10, 90%) had neutralizing antibodies. Most patients (41/54,76%) and all siblings (13/13) had still a significant T-cell response against CoV2-protein S. Twenty-six documented infections occurred between D0 and M6: 22 infections in patients and 5 in siblings. The number of infections was not statistically different between the two groups. No severe infections were reported. In patients, 15 infections resulted in a delay of chemotherapy from 5 to 14 days.
Conclusion: A vaccination regimen with 2 or 3 doses of 30µg of BNT162b2 vaccine was well tolerated and resulted in a significant and prolonged humoral and cellular response in most children with acute leukemia while completed following the most intensive chemotherapy period. These results show that children with acute leukemia are able to respond to RNA vaccines. Utilizing these vaccines for antitumor purposes to prevent relapse should be further explored.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal